H5N1 Influenza: A Growing Threat or a Contained Risk?
46 Cases Across Six States. Is H5N1 the Next Pandemic Threat?
Over the past two decades, the H5N1 avian influenza virus has hovered on the edges of public health consciousness, occasionally surfacing as a potential pandemic threat. Recent developments, however, have reignited concerns among epidemiologists and virologists. With a growing number of human cases, increasing host range, and concerning mutations, the question lingers: Could H5N1 spark the next global pandemic?
What is H5N1?
H5N1 is a highly pathogenic avian influenza virus first recognized in humans in 1997. While predominantly infecting birds, recent cases have demonstrated its ability to spill over into mammals, including humans. The current dominant strain, clade 2.3.4.4b, emerged in 2021 and has since spread globally via migratory birds (Webby & Uyeki, 2024). Alarmingly, it has now been detected in species like marine mammals, dairy cows, and humans (CDC, 2024).
H5N1 Infections in Humans: A Growing Concern
Since 2003, over 900 human cases of H5N1 have been reported across 24 countries, with a staggering case fatality rate of 50% (El-Shesheny et al., 2020). However, this reported fatality rate may not reflect the true mortality burden of the virus, as milder infections often go undetected or unreported. In the United States, H5N1 cases have increased in frequency and geographic spread since 2024, linked to outbreaks in poultry and dairy farms. Most reported cases in the United States have been mild, with symptoms such as conjunctivitis (observed in 93% of cases), fever (49%), and respiratory symptoms like cough or sore throat (36%). The median illness duration was four days, and none of the patients required hospitalization or died (Ison & Marrazzo, 2024). However, severe cases, such as a teenager in Canada who required extracorporeal membrane oxygenation, underscore the virus's potential for virulence (“Critical Illness in an Adolescent With Influenza a(H5N1) Virus Infection,” 2024).
Human infections are primarily occupational, occurring during exposure to infected animals or contaminated environments. However, the use of personal protective equipment (PPE) among exposed workers has been inconsistent. For instance, only 36% of U.S. workers used both eye protection and masks, despite the virus being detected in conjunctival swabs in 88% of patients (Ison & Marrazzo, 2024).
Why is H5N1 Concerning?
Recent findings suggest H5N1 is closer than ever to becoming a pandemic threat:
Mutation Potential: Studies have shown that a single amino acid mutation (Gln226Leu) could enable H5N1 to bind more effectively to human cell receptors. This mutation has already been observed in laboratory settings (Lin et al., 2024).
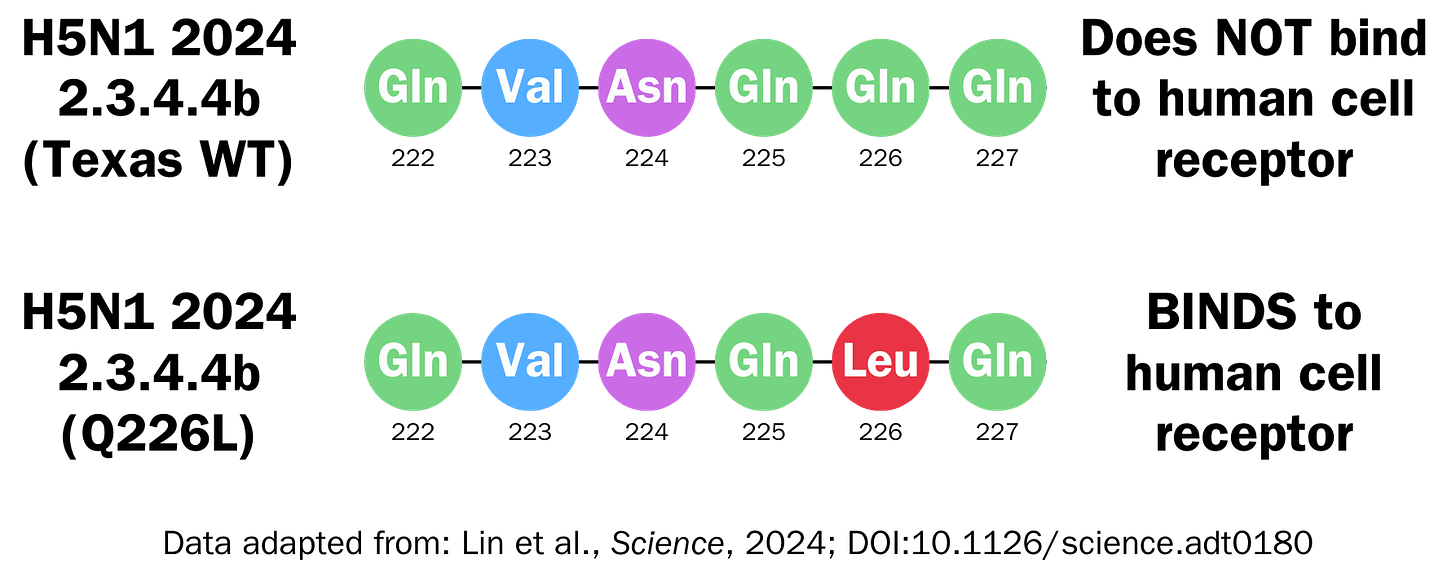
Image by Bryan Cobo for The Public Eye. Data adapted from Lin et al., Science, 2024. In the image, the mutation Gln226Leu is shown with the single letter abbreviation as Q226L. Expanding Host Range: H5N1 has infected diverse species, increasing human exposure and opportunities for the virus to adapt (Butt et al., 2024).
Undetected Spread: Evidence of asymptomatic human cases suggests the virus may be more widespread than current surveillance indicates (Garg et al., 2024).
Understanding the Public Health Impact of H5N1
Despite these red flags, sustained human-to-human transmission has not yet been observed. Historical precedents like H7N9, which raised similar alarms but failed to cause a pandemic, offer a note of cautious optimism (Kupferschmidt, 2021). However, experts warn against complacency. Dr. Michael Osterholm, a leading infectious disease expert, likens the virus's evolution to “a key that sits in the lock, but it doesn’t open the door”: the right sequence of mutations could unlock its pandemic potential (Ungar, 2024).
Can We Prevent Another Pandemic?
Preparedness is our strongest defense. Here’s what experts recommend:
Enhanced Surveillance: Monitoring mutations and geographic spread is critical for early intervention (Maxmen & Allen, 2024).
Vaccine Development: While stockpiles of H5N1 vaccines exist, they may not match evolving strains. Innovations like mRNA vaccines could offer faster, more targeted solutions. (Fox, 2024)
Public Trust: Lessons from COVID-19 show the need for clear communication to counter misinformation and foster compliance with public health measures (Feltman et al., 2024).
Should We Be Worried?
The answer lies in vigilance rather than fear. As Seema Lakdawala, a flu researcher at Emory University, notes, "If H5 is ever going to be a pandemic, it’s going to be now." Yet, as other experts remind us, the virus’s path is unpredictable (Wilcox, 2024).
While H5N1 presents a formidable challenge, the world is not defenseless. With robust surveillance, scientific innovation, and global cooperation, we can mitigate its risks and safeguard public health.





